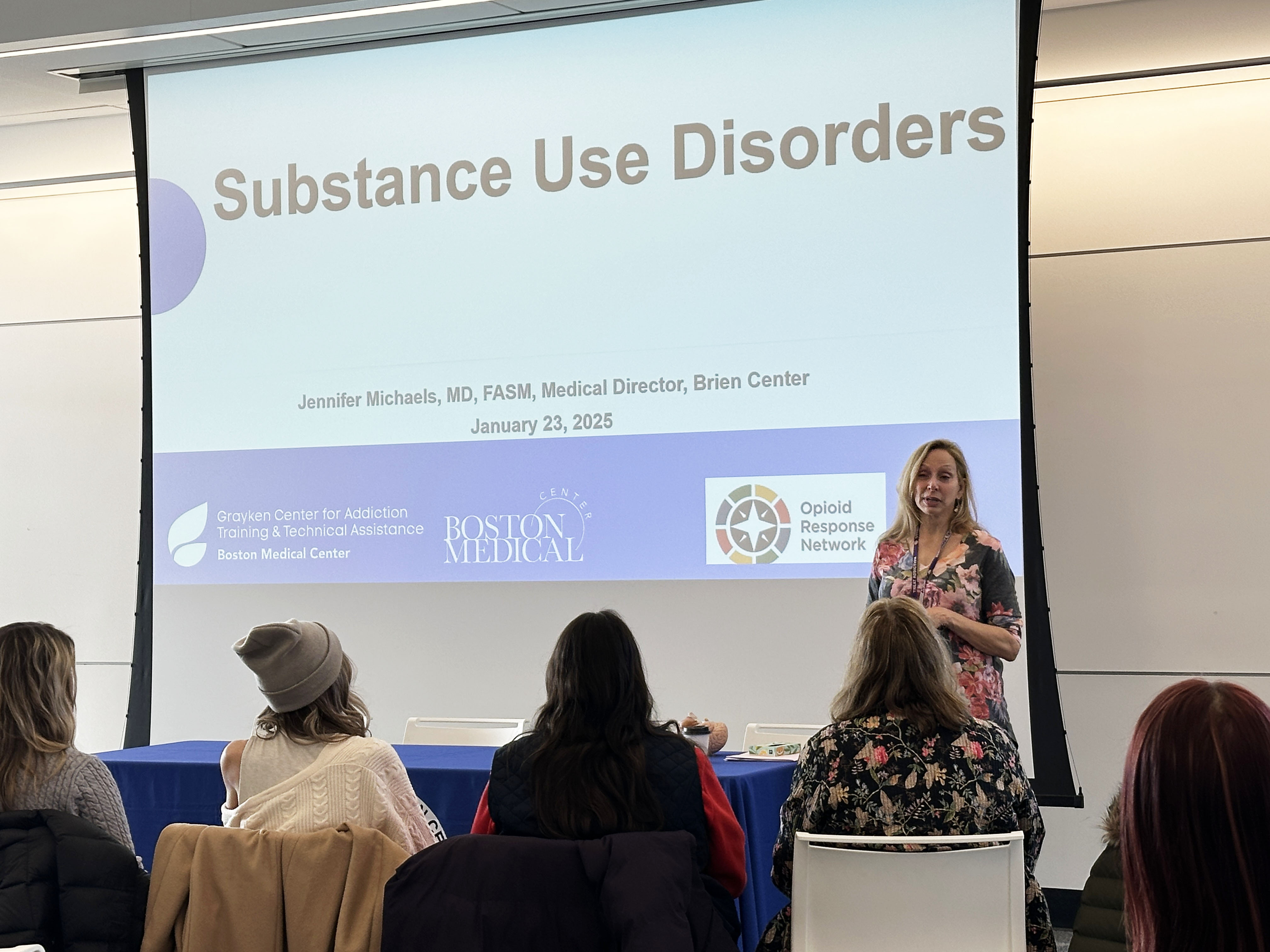
When navigators expressed the need to better understand substance use disorders and treatment options in Berkshire County, Berkshire United Way and the navigation convening committee connected with professionals in the field to present on this topic recently.
Panelists included Dr. Jennifer Michaels, medical director for The Brien Center; Sarah DeJesus, program manager for Berkshire Harm Reduction; Andy Ottoson from Berkshire Regional Planning Commission (BRPC); and Andrew Walak, program manager for Berkshire Clinical Stabilization Services (CSS).
Providing an overview of substance use disorders, Dr. Michaels shared that current trends with substance use are showing more use of Fentanyl, stimulants, and Xylazine and Medetomidine, both used in the veterinary field. And according to the most recent data available, from 2015 to 2021, there was an uptick in overdose deaths connected to Fentanyl and Methamphetamine use.
The work that’s being done today – the services and resources that are available, especially in Berkshire County – we didn’t see as much 10 years ago, said Dr. Michaels. “The fact that we’re meeting here today is innovation.”

A 135-page analysis of the substance use disorder landscape in Berkshire County confirms there is a strong infrastructure in place to address the lifecycle of prevention, harm reduction, treatment, and recovery. This analysis is the result of decades of hard work and includes a lot of resources, said Andy, who co-facilitates substance misuse prevention and overdose reduction programs for BRPC through the Berkshire Overdose Addiction Prevention Collaborative.
Dr. Michaels emphasized that substance use disorder is a chronic brain disease that attacks the reward center of the brain but is treatable. The recovery process is a continuum of care, she said, with most people landing in outpatient services. Evidence-based medications work but aren’t being used because they are stigmatized. These medications, as well as evidence-based psychotherapies, can help stop chronic use. She also said that community outreach, peer support, and self-help groups are beneficial throughout this recovery process.
Dr. Michaels offered this takeaway: the key to successful treatment is immediate access to evidence-based treatments for all and learning the facts. This is where Berkshire Harm Reduction comes in.
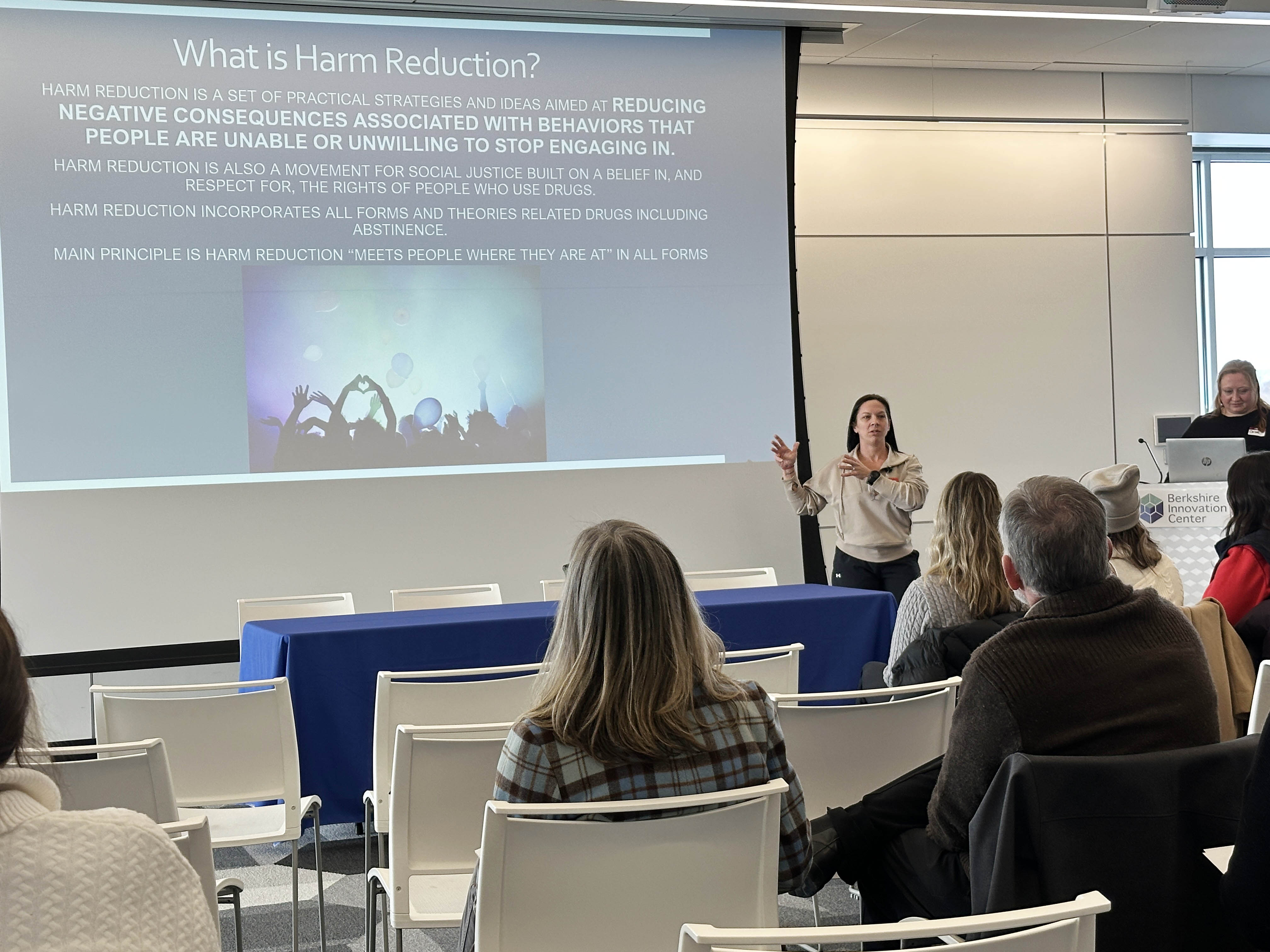
Associated with Berkshire Health Systems (BHS), Berkshire Harm Reduction aims to educate the public about drug use and mitigate health complications. Harm reduction is associated with major treatment or boots on the ground. There are prevention programs and treatment programs and “a lot of people are in between these two programs,” said Sarah.
Berkshire Harm Reduction has expanded its community outreach over the last several years, more recently and noticeably providing public access to Naloxone and vending machines stocked with additional harm reduction supplies. “These are an extension of our services to keep people safe,” she said. Community outreach is “part of that continuum of care.”
Clinical stabilization services are a significant step in the recovery journey. Andrew described Berkshire CSS as an inpatient, three-story housing unit in Pittsfield that currently offers 24 beds, with one ADA compliant room on the first floor. Males and females are separated by floors and must be 18 or older.
Berkshire CSS has recovery specialists, a counseling team, and can provide transportation and interpretive services in any language through BHS. He said there is an intake line but there is often a waitlist; priority is given to patients receiving behavioral or mental health services through BHS. They take most insurances and even with no insurance, they will work it out.
Andrew said a high rate of people going through the 14-day program complete it. If they can’t get a bed here, program coordinators will try to find a location of preference. “We have two coordinators who know the system well,” he said. In response to a question, he said many patients come back, but it’s a wait. In response to another question, he noted that patients can enter the program only after detox.
Katherine von Haefen, BUW director of Community Impact, asked the panel about guidance for our community navigators. John Crane with The Brien Center suggested peer-to-peer networking – reaching out to recovery navigators.
“This time together is always in service of providing navigators with information and resources they need to best help folks in the community. This session provided them with critical information on substance use disorder, and with this knowledge comes the power for navigators to better serve families and individuals, including how to make effective referrals for various treatment options,” said Katherine.
The next convening on February 28 at the Berkshire Innovation Center will focus on best practices and will be led by Katrina Mattson, Tapestry Health’s health services manager.
